People from all ages, occupations, and sport disciplines complain of low back pain. A tight Psoas often contributes to your back pain. Good News? You can avoid it… you can even fix it.
Where and What is My Psoas?
The Psoas is one of the largest and thickest muscles in the body. It attaches to the vertebrae of your lower back, and the head of your femur (thigh bone). The Psoas is primarily responsible for hip and thigh flexion and has a lot of influence over your lumbar posture and the way your hips are positioned.
When you’re sitting for a prolonged period of time, your Psoas is in a shortened position. Leave it for long enough, and it will start to think this is normal. Your tissues want to move into that resting position. Leaving you tight & contracted.
Incorrect posture during standing and walking (which is often caused by a tight Psoas) will leave it even tighter and harder to loosen.
Why Does It Cause Back Pain?
A tight Psoas is a killer for your back for various reasons.
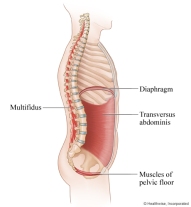
If it is tight and in a contracted state, your Psoas will want to bring your lower back forward, moving you into an anterior tilt: lordotic posture.
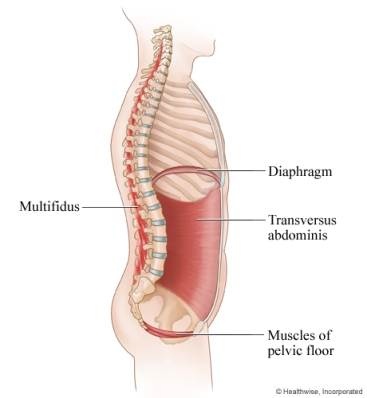
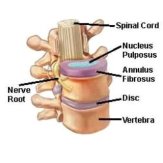
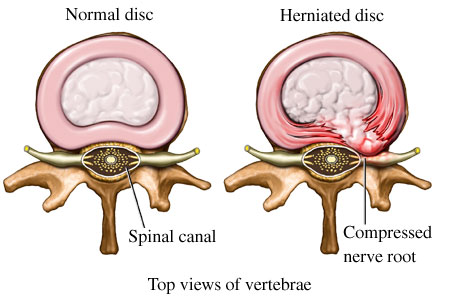
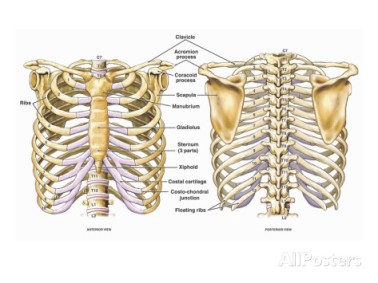
The pressure exerted by the Psoas whilst in a contracted state can compress the joints and discs of the lumbar vertebrae. This pressure causes degeneration and will make them more susceptible to injury.
A shortened Psoas on one side will pull the spine or pelvis to that side, leading to many painful problems, including scoliosis.
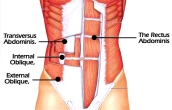
A tight Psoas will stop your Glutes firing and activating normally. This is Reciprocal Inhibition: the Psoas and the Glutes are opposing muscles.
Lack of Glute activity plus horrific posture can lead to overcompensation in other muscles of the back, leaving them tight and overworked. Couple this with the referring pain from the trigger points in your Psoas and you will be hurting.
Tips to Avoid A Tight Psoas.
There are several ways to stop your Psoas turning into a hazardous plank of wood. All of which are easy to implement and should be even if you don’t suffer from back pain yet. Here goes…
Postural Corrections. If we stay in a certain position all day, our tissues will want to move into that resting position, in this case, your Psoas. The best sitting posture is one that always changes.
Sit Back in Your Chair. This will stop you leaning forward as much, and thus your Psoas won’t be in as shortened position in comparison to when you sit on the edge of your seat.
Stop Hooking Your Feet under Your Chair. You put yourself in more hip flexion and therefore, more Psoas activation. Set your feet flat on the floor, or a raised platform if you are a shortie.
Stand Up When Performing Exercises. You sit all day at work and keep your Psoas shortened. Do the opposite in the gym. Instead of the bike, get on the treadmill. Sub in Overhead Press instead of Seated Press.
Stop Sleeping on Your Stomach. When you are on your stomach, your back goes into hyperextension. This is exacerbating what a tight Psoas already does to your back (anterior tilt). Change it up.
Move More. Not staying in a seated position all day will go a long way to stopping you developing a tight Psoas. Get up more frequently, stretch more often, change positions… just keep moving!
Tips To Loosen A Tight Psoas.
If you do suffer from low back pain and you suspect a tight Psoas, relax (maybe your Psoas will follow the lead), read the next few tips, and get cracking.Stretch. Add Psoas and Hip Flexor stretches after your workouts. Get out of your chair at work occasionally and do some stretches. Do some at night before you go to bed. You can do this one:
PSOAS STRETCH ATTEMPT
The most effective way to loosen your Psoas is through a therapist.For more information about Kinetic Physiotherapy, visit our website:http://www.kineticphysiotherapy.ca Contact Kinetic Physiotherapy via e-mail:info@kineticphysiotherapy.ca or phone: 905-637-1414 to set up an appointment.